Kayla first tried fentanyl when she was a troubled 18-year-old in North Carolina.
“I literally felt amazing. The voices in my head went completely silent. I was immediately addicted,” she recalls.
The little blue pills Kayla became addicted to were likely manufactured in Mexico and then smuggled across the border into the United States, a deadly trade that President Donald Trump is trying to end.
But drug cartels are not pharmacists. Kayla never knew how much fentanyl was in the pills she used to take. Did they have enough synthetic opioid to kill her?
“It’s scary to think about,” Kayla says, reflecting on how at any moment she could have overdosed and died.
In 2023, there were more than 110,000 drug-related deaths in the US.
At that time, the advance of fentanyl, 50 times more powerful than heroin, seemed unstoppable.
But then a surprising change occurred.
In 2024, the number of overdose deaths in the US will be reduced by approximately 25%. This means almost 30,000 fewer deaths: dozens of lives saved every day.
Kayla’s state, North Carolina, is at the forefront of this trend.
Why have fatal overdoses fallen so dramatically?
One of the reasons for this trend is the commitment to reduce the harm caused by drugs.
This means promoting policies that prioritize the health and well-being of drug users rather than criminalizing these people, recognizing that, in the era of fentanyl, drug use often results in death from overdose.
In North Carolina, where Kayla still lives, overdose deaths have decreased by 35%.
There the strategy is well developed.
Kayla no longer uses illicit drugs. It is part of an innovative assisted-tracking program, known as LEAD, in the upstate city of Fayetteville.
This program is a collaboration between the city police and the North Carolina Harm Reduction Coalition, who work together to keep drug users away from crime and toward recovery.
“If we see someone shoplifting at a grocery store, we check their criminal record. We often find that the crimes they commit appear to fund their addiction,” explains Lt. Jamaal Littlejohn.
This could make them candidates for the LEAD program, where they get support to address their addiction and so they can start thinking about getting secure housing and employment.
Proponents of the LEAD program say it’s not about going soft on crime: Drug dealers still go to jail in Fayetteville.
“But if we can get people the services they need, law enforcement will have more time to deal with major crimes,” argues Lt. Littlejohn, who watched his own sister struggle with substance abuse.
“You’re still playing Russian roulette, but your odds are getting better”
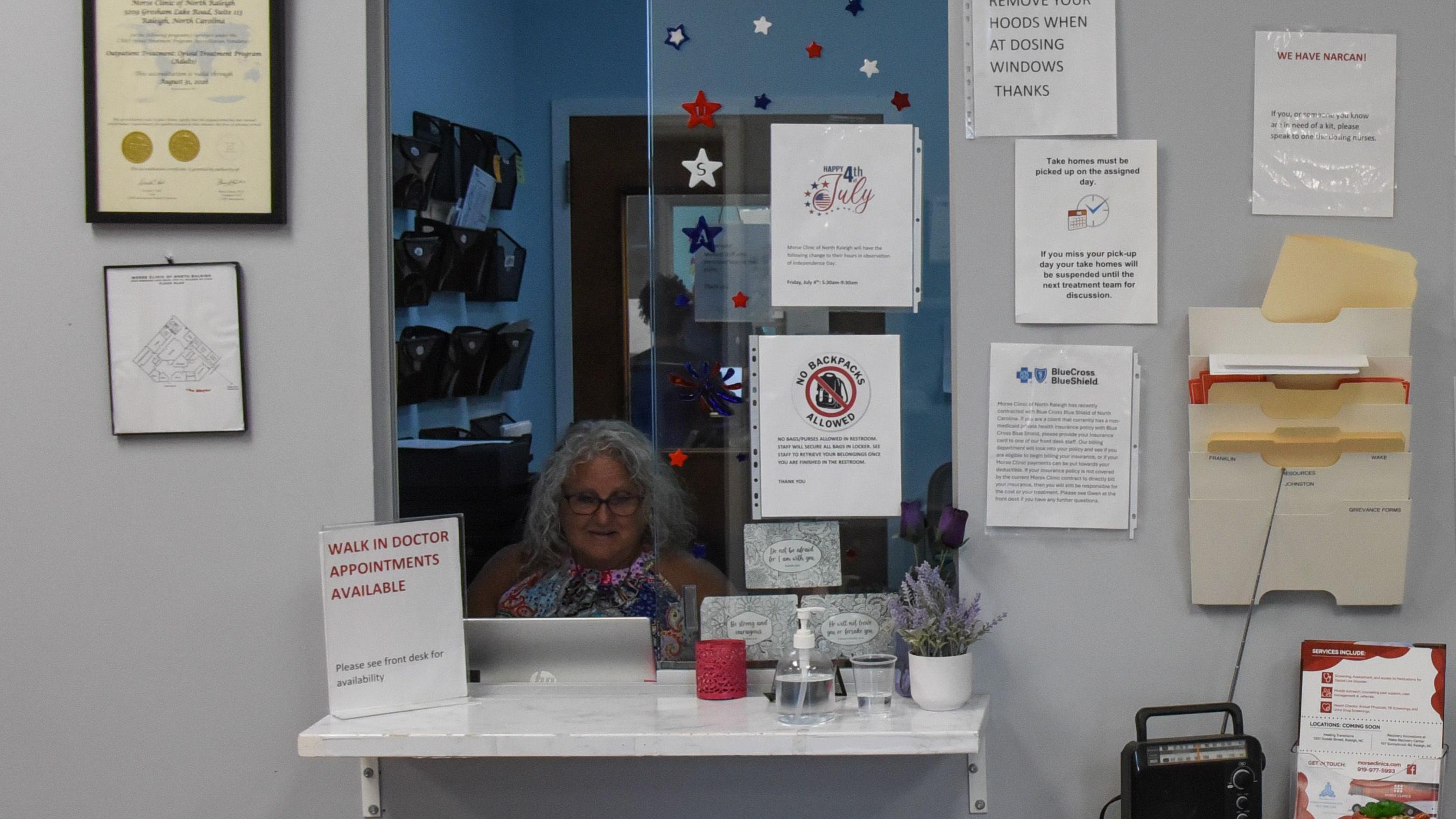
At 9 am, at one of the Morse clinics in the state capital, Raleigh, 2 or 3 people wait their turn at the reception.
“The busiest time is 5:30 a.m. to 7 a.m., which is before work,” says Dr. Eric Morse, an addiction psychiatrist who runs nine medication-assisted treatment (MAT) clinics in North Carolina.
“Most of our patients work; once sober, they arrive at work on time every day.”
The clinic has an impeccable management system. After registering, patients go to a dosing window where they receive their dose. They come and go in a matter of minutes.
They are given random drug tests for illicit narcotics. Dr. Morse says about half of his patients still test positive for street-bought opioids, but he doesn’t consider it a failure.
“Maybe you use once a week and you’re used to using it three times a day… You’re still playing Russian roulette with fentanyl, but you’ve taken a bunch of bullets out of the chamber, so your survival rate increases significantly,” Morse explains.
This is known as harm reduction.
So, instead of being kicked out of the treatment program, patients who test positive for drugs receive more support and counseling.
Dr. Morse claims that 80% to 90% will stop using illegal drugs completely. And over time, many will also gradually reduce the dosage of the medication.
The debate over abstinence

Not everyone thinks this is the right approach.
Mark Pless, a Republican member of the North Carolina House of Representatives who worked as a full-time paramedic, says illicit drug use begins with a decision.
He doesn’t believe in harm reduction. In particular, he opposes treating opioid use disorder with medications such as methadone or buprenorphine.
“You are replacing an addictive product with another addictive product,” he says.
“If you have to take it to stay clean, it’s still addictive. We have to find a way for people to get better; we can’t leave them dependent on drugs forever.”
He favors abstinence programs, when drug users stop using cold turkey.
But many health care professionals in North Carolina have concerns about this method.
“I believe there are multiple paths to recovery,” says Dr. Morse. “I do not discount abstinence-based treatment, except when the medical evidence is analyzed.”
Dr. Morse refers to a 2023 Yale University study, which looked at the risk of death for opioid users in a treatment program, compared to those not receiving it.
The study suggested that a person in withdrawal treatment was just as likely, or even more likely, to die from an overdose than a person not receiving withdrawal treatment and continuing to use over-the-counter opioids like fentanyl.
Treatments aside, there is another medication that is helping to alleviate the crisis.
Naloxone is widely available and, in nasal spray form, reverses the effect of an opioid overdose, helping the person breathe again.
In North Carolina, as of 2024, it was administered more than 16,000 times. This represents potentially 16,000 lives saved, and this number only includes overdose reversals that have been reported.
“This is as close to a miracle drug as we can imagine,” says Dr. Nabarun Dasgupta, a street drug scientist at the University of North Carolina.

Many users of narcotics such as cocaine, methamphetamine, and heroin want to be sure that what they are using is not going to kill them.
Some people use test strips to test for fentanyl because they know the drug is linked to many overdose deaths.
But these strips do not identify all potentially harmful substances.
Dr. Dasgupta runs a national drug testing laboratory. Users send a small portion of their drug supply to him through local nonprofit organizations.
“We have analyzed nearly 14,000 samples from 43 states in the last 3 years,” he says.
A generational change
Testing drugs for potentially dangerous additives is an additional weapon in harm reduction.
Dr. Dasgupta believes another reason for the decline in overdose deaths in the U.S. is that young people are avoiding opioids like fentanyl.
“We’re seeing a demographic shift. Young people from Generation Z die from overdoses much less frequently than their parents’ or grandparents’ generations did when they were the same age,” he says.
Dr. Dasgupta isn’t entirely surprised that 20-somethings are avoiding opioids.
Alarmingly, four in ten American adults know someone whose life ended due to an overdose.
It was this epidemic of death, started in the 1990s by prescription opioids, that motivated North Carolina’s former attorney general, now the state’s governor, to act against the powerful corporations that profit from the dark spiral of addiction of so many Americans.
Josh Stein telephoned his counterparts in other states and took a key role in coordinating legal actions against opioid manufacturers, distributors and retailers.

The result, after years of intense negotiations, was an Opioid Agreement totaling about $60 billion.
This money, which large companies have agreed to pay to US states, will go toward “reducing the opioid epidemic.” North Carolina’s share is about $1.5 billion.
“You have to invest it in four ways: drug prevention, treatment, recovery and harm reduction. I think it’s transformative,” says Governor Stein.
Meanwhile, funding from the national government is uncertain. The cuts to Medicaid included in President Trump’s One Big, Beautiful Bill could have a tremendous impact in this area.
At Morse Clinics in Raleigh, 70% of patients rely on Medicaid. If they lose health insurance, will they stop treatment and become more vulnerable to dying from overdose?
Although drug mortality statistics in North Carolina appear optimistic, thousands of people continue to die, and the state’s Black, Indigenous, and non-white populations have not experienced the same rates of decline.
And there are other states that have seen a stubbornly slower pace of decline in fatal overdoses, including Nevada and Arizona.

Nobody gives up. And even less Kayla.
Under the influence of fentanyl for three long years, he never overdosed, but he did have to save his friends.
Kayla’s parents didn’t know what to do with her.
“They kind of gave up on me; they thought I was going to die,” he recalls.
Kayla recognizes the contribution of Charlton Roberson, the mentor who helped in her recovery. His goal now is to gradually taper off methadone and become drug-free. He also wants to find a job in a hospital.
“I feel more alive than when I used fentanyl,” she says.
Keep reading:
* DEA alerts about nitazene, a deadly drug 100 times more powerful than fentanyl found for the first time in New York
* UN warns of the danger of fentanyl variants in the US.
* Stress, pain and fatigue: Which professions are most linked to fatal overdoses in New York?
click here to read more stories from BBC News World.
Subscribe here to our new newsletter to receive a selection of our best content of the week every Friday.
You can also follow us on YouTube, Instagram, TikTok, X, Facebook and on our channel WhatsApp.
And remember that you can receive notifications in our app. Download the latest version and activate them.

